Issues Surrounding Proton Therapy
Some technologies have been so superior that they were immediately put into use. Invented in the 19th century, x-rays represented the first time doctors could look inside the body without cutting it open. They first used x-rays to locate shrapnel in war wounded, indicating where to operate. Within a year, x-rays were available around the world. No scientific studies required or performed.
Similarly, high-tech iterations of x-rays have gone from invention to marketing to immediate use without further ado. Robotic surgery sprang onto the scene without a sheaf of scientific studies. In fact, the vast majority of medical technologies and procedures prevalent today never underwent actual scientific scrutiny.
Proton therapy represents the first type of radiation that stops at the target and avoids damaging most healthy tissue. I find it just as revolutionary as any of the other technologies rushed into use without further study. However, critics of proton therapy demand that before it can be justified (because of its cost) there must be decades of highly expensive scientific trials to verify its efficacy. This double standard smells of a ploy by radiologists to protect their own turf.
Proton therapy began 70 years ago and cannot be called new, investigational, or unproven. Every proton therapy center tracks its patients and accumulates statistics regarding their success rate. Further, many prospective trials exist, following a group of subjects over time to document their experience. I am in such a trial for the rest of my life, a Medicare registry.
Even studies that directly compare proton therapy to other modalities, especially x-rays, showing the superiority of proton therapy, are rejected as being anecdotal and not randomized, double-blind, and peer-reviewed. The type of studies demanded, besides costing millions of dollars, bring up serious ethical issues. As an example, consider a test of parachute designs. Would you allow people to risk their lives jumping out of airplanes with potentially inferior parachutes, that may lead to their injury or death?
The same principle applies to proton therapy. Requiring one group of patients to accept inferior treatment to amass statistics violates the medical imperative to do no harm. Diagnosed with prostate cancer, my wife’s cousin rejected a chance to participate in a trial comparing x-rays and protons. Since each group got picked randomly as to their modality, he declined, not wanting to risk getting assigned to the x-ray group.
Despite the pitfalls and difficulties, a well-financed highly technical trial undertaken by fifty medical institutions may give the definitive answer to x-rays and protons for prostate cancer. Their impressive website shows the vast extent of their efforts (see www.comppare.org)(yes, there are two p’s).
Insurance companies, in their effort to avoid paying for the higher cost of proton therapy, have switched their strategy from calling it unproven and experimental to claiming lack of medical necessity. Other modalities, they say, work just as well (at a lower cost). Frankly, they don’t care if you wear diapers the rest of your life, or if the cancer may come back. Some studies show the shortsighted nature of this policy, as the total cost of treatment, including treating the side effects and further complications such as secondary cancers, adds up to more than proton therapy would have cost to begin with.
Fortunately, patients need not fight this battle, as they can choose proton therapy at 40 proton centers in the United States and more around the world. And, increasingly, insurance companies agree to coverage (see INSURANCE). However, other bumps in the road have slowed the progress and acceptance of proton therapy, some of which I detail in this essay. You will find this essay longer than any of my others because I think the subject warrants your attention.
COMPETITION
Radiologists find themselves in a difficult spot. If they admit the superiority of proton therapy, then ethically they should refer many of their patients to proton therapy centers. How, then, could they make a living? Therefore, many of them continue to publish or read articles designed to assure themselves that x-rays offer similar results, or even superior.
I gave a talk about proton therapy describing how protons avoid unnecessary collateral damage, especially it areas such as the brain. Afterwards, a man came up and told me when his oncologist found a brain tumor, he sent him to a radiologist at MD Anderson in Houston. Treated with traditional x-rays, the man experienced significant cognitive damage. He asked, “Why didn’t they tell me about proton therapy if they have it at MD Anderson?”
Why? Because radiologists will unethically sell out patients in order to make a living. (More about this toward the end of the essay.)
Of course, sometimes x-rays qualify as the best treatment. A specific protocol exists to evaluate patients and assign them to the best modality. That being said, I have a better solution for radiologists. Rather than subjecting your patients to inferior treatments, go to work at a proton therapy center. As the industry grows, centers constantly seek qualified staff. Be part of the answer not the problem.
COST
Because the promise of proton therapy led to high estimates of demand, the first centers typically had three to five treatment rooms and cost as much as $200 million. One estimate stated proton centers cost 40 times as much to build as x-ray facilities. Perhaps being “only” twice the cost qualifies as a pretty good deal. Cyclotrons weighing fifty to one hundred tons come from Belgium by boat and then via highway in special convoys with custom-built 48-wheel trailers.

Above: Delivery of the cyclotron to Knoxville, TN, went across the ocean, up various rivers on barges, and then by highway, taking up all lanes.
One company in California initiated the construction of five proton centers at exorbitant costs evidently planning to make a killing. One center went bankrupt before completion, never to be completed. The other four eventually went bankrupt or engaged in financial reorganization. New operators who bought the centers out of bankruptcy have a much lower overhead and can operate in the black. They went through a rough start.
The cost of building a proton facility means that only the largest institutions or alliances can undertake such projects. The Mayo clinic raised the money to pay cash for its two $180 million centers. As a result, it charges the same for proton therapy as for x-rays. Several other centers have the same pricing guidelines. Going there may convince insurance companies to pay for the treatment (see INSURANCE).
In an article called “Three Ways to Make Proton Therapy Affordable” (https://www.nature.com/news/three-ways-to-make-proton-therapy-affordable-1.22660) authors Thomas R. Bortfeld and Jay S. Loeffler make this statement:
If cost was not an issue, proton therapy would be the treatment of choice for most patients with localized tumours.
Further, total cost must include any expense for side effects or recurrence subsequent to treatment. In one case, a young child with a medulloblastoma (brain cancer) successfully treated with conventional radiation therapy had a soft tissue sarcoma develop three years later at the site where the radiation exited his body. "Had they treated the patient with PBT (proton beam therapy), they would have avoided any exit radiation and the family would not be battling a second life-threatening cancer," the doctor said. "In cases like that, I don't think you can measure the cost of PBT in dollars and cents."
Even though cost remains an issue, don’t give up hope. Recent developments have lowered the cost of building proton centers considerably with the hope the treatment cost will follow suit. (See: FUTURE)
BAD PRESS
Radiology journals have published many negative articles regarding proton therapy. Doctors perusing only the headlines could easily conclude that protons did not provide sufficient value for the cost and pass that opinion to their patients.
Journalists hoping for a big scoop write articles calling proton therapy a needless medical arms race, beating the dead horse of excessive cost and lack of scientific proof. Striving to be unbiased, many authors sought something negative to balance all the positives. One particularly obnoxious frequently quoted opponent of proton therapy until recently worked at Harvard. He called proton therapy the doom of our health system, the prime example of irresponsible spending, and worse. (Ironically research at Harvard developed proton therapy as a medical treatment.)
The bankruptcies led journalists to write articles calling proton therapy a fad, a bubble, an attempt for status. They called out proton centers for hype over promising what proton therapy can do. All of this has led to a rocky and unrepresentative relationship with the public.
ASTRO, a leading and very influential organization of radiologists provides suggested standards for the United States government, hospitals, and insurance companies. In my mind they have deliberately sabotaged proton therapy. As a result, one government committee put out an annual report saying very negative things about proton therapy. A proposed change in Medicare payments, again based on suggestions from ASTRO, made no special accommodation for proton therapy, saying all radiation should cost the same. Fortunately, before financially crippling many canters, the Biden administration delayed this policy that hopefully will not see the light of day.
Akin to bad press is no press. I went to a big ASTRO convention in San Antonio and picked up a copy of each of their brochures about cancer treatment. Most of them gave one sentence (a paragraph at most) to proton therapy, saying that it might affect less healthy tissue. Later in the booklet, several pages described how to deal with the common side effects of x-rays. At least one booklet didn’t even mention proton therapy.
I should say that doctors working with proton therapy are also radiologists, some of them members of ASTRO, and all the largest proton equipment manufacturers display their wares in expensive booths at ASTRO conventions. They have not totally shunned proton therapy, just treated it like a second-class citizen. But that will change.
Proton therapy is not some kind of alternative fringe treatment. Mainstream medical organizations with big bucks are behind it. That being said, several bankruptcies left the initial investors holding the bag. Even Provision, the center where I went for treatment in Knoxville, went bankrupt in 2021, now renamed Thompson Proton Center. (Disclosure: I own stock in IBA, the world’s foremost proton therapy equipment maker in Belgium. I consider it a gesture of support, as the stock has not done well.)
Of course good press also exists. Many articles praise proton therapy for its unique capabilities. I originally intended to state their arguments in my books so as to rail against them but decided against it, not wanting to give them even more coverage. Let them write their own books.
Go to any working proton therapy center and you will find truly inspiring healing happening there every day. The bumps in the road did not blockade the route, only slowed it down a bit. Cream rises to the top, as they say, and proton therapy will have its rightful place in the sun.
To avoid fraudulent claims, search for your particular type of cancer on a respectable website, such as PubMed, a database of the National Institute of Health (https://www.ncbi.nlm.nih.gov/pubmed/). For example, search under “breast cancer and proton therapy.” You will find many articles that give the results of actual trials and studies. Even then, you may need to be cautious, because the design of the trial may be such as to guarantee a particular outcome. I discuss a particularly egregious example of this in a lengthy example at the end of this essay.
UNFAMILIARITY
Your family doctor, urologist, or even your oncologist may not be familiar with proton therapy much less well-versed. No doubt they continue to prescribe x-rays and surgery for their patients as they have always done. If challenged, they say they have the patient’s best interest at heart. I have made it clear on this website that you cannot depend on the advice about proton therapy from your doctor.
With only 40 proton therapy centers in the United States, chances are high that most people have not run across it before. San Antonio, where I live, supports many thriving medical establishments, some grouped in areas like the Medical Center. Even though we rate as the seventh largest city in the United States, only now is one of the main health providers building a single gantry proton therapy facility. Several favorable segments have made it to the evening news. Yet you can’t expect people not yet facing a medical diagnosis to remember something as esoteric as nuclear medicine.
Flying Southwest Airlines, I have on a number of occasions noticed Love Field in Dallas displays electronic billboards touting the local proton center. The internet serves as the initial source for many people researching cancer treatment. Hence my site.
Even if the medical world won’t heartily embrace proton therapy, knowing patients themselves will demand it.
In 2015, MEDRays Intell Proton Therapy World Report called for 300,000 patients to be treated annually with proton therapy by 2030, only eight years from now That would require sixty new centers. For two years running, MEDRays downgraded their estimate for the growth of proton therapy centers by twenty percent, not due to lack of need, but lack of demand. Those statistics reflect the effects of the bumps in the road described in this essay.
I hope, as an advocate for proton therapy from the patient’s point of view, to bring attention to proton therapy just enough that those not familiar with it will take it upon themselves to look further. Word of mouth. Personal recommendation. Discussion at support groups. Social media. As patients, we can help give proton therapy a boost.
INSURANCE
Although improving, the difficulty in getting proton therapy covered by insurance remains a big bump in the road, creating a Catch-22 situation. Insurance companies demand more studies and more data before they cover proton therapy. However, in order to get patients into the trials, they need to receive the treatment, which means coverage by insurance companies. Some insurance companies may cover proton therapy if you participate in a trial. A doctor at the Mayo Clinic put it like this:
"We're not going to be able to conduct these studies if we don't have buy-in from payers. We can't execute clinical trials in this country for radiation therapy without the cooperation of the insurance carriers.” Good luck with that.
The “rules of evidence” demanded of random trials do not fit proton therapy very well, as protons are superior largely for what they don’t do, namely they avoid damaging healthy tissue and causing side effects.
Insurance companies should fight cancer, not their clients. For pediatric cases under 21 years old, most insurance companies agree to cover proton therapy. Medicare covers those over 65 for most types of proton therapy. It boggles the mind, then, that insurance companies continue to claim proton therapy is unproven only for people between the ages of 21 and 65. For more on insurance, see: (INSURANCE).
TIME
A time will come when proton therapy will be a mainstream treatment, respected for its results, recognized by the public, affordable, referred by doctors and covered by insurance. It just takes time. Some new medical technologies took 50 years to reach full acceptance. Thirty years down and two more decades to go.
Time matters to patients as well. Delays in availability, in proper diagnosis, or battles with insurance companies, come with a risk that the cancer may get worse. I met a man who fought Cigna for many months, finally getting coverage, but he died two months later. Earlier treatment may have saved his life.
During my research phase, I called MD Anderson to ask some questions, left an urgent message, and never received a callback. I guess they are so famous that they have all the business they can handle. Indeed, they are currently expanding to double their capacity for proton therapy. I suspect patients may need to queue up and wait for an availability.
Time tempers the initial cost of most new technologies. Advances and popularity combine to lower costs and increase availability. Time also matters in prospective trials, measuring results for five years or more. Five years’ survival from cancer rates as a success, although my wife Ruth, who died after six years with breast cancer, would certainly not see it that way.
In time, proton therapy centers will run at full capacity. In time, the critics will fall away, their dire predictions relegated to the dustbin. In time, some spectacular advances will become available, such as one session FLASH treatments. (See FUTURE)
Stereotactic Body Radiation Therapy (SBRT), an x-ray technology, stresses how few treatments their protocol requires, typically ten days whereas both of my proton treatments took seven weeks. Especially if you must travel to receive your proton therapy in another city, away from family and work, time becomes a burden. Happily, trials have shown that hypofractionated protocols (fewer sessions at a higher dose) work equally well with proton therapy as x-rays. Fewer sessions should also bring down the cost of the treatment.
PROTON CRITICS CLING TO FLAWED STUDY
Thanks for reading this far. Below I go into detail to show how a study widely touted in favor of x-rays (with headlined articles in medical newsletters) actually proved just the opposite.
An article in MedPage Today heralded the results of the trial with the headline: “No Reduced Toxicity for Proton Tx vs IMRT in NSCLC.” Proton Tx stands for proton treatment. IMRT means Intensity-Moderated Radiation Therapy, a type of x-ray treatment. NSCLC stands for Non-Small Cell Lung Cancer.
Strangely, the misleading aspects of the study come mostly from its poor design, even though conducted by MD Anderson and Massachusetts General Hospital, both of which have proton centers.
Because lungs move during treatment, they can be subject to inaccuracies that lead to a common side effect known as pneumonitis. The study did not focus on how well the two modalities killed cancer, assuming, I suppose, that they performed equally in that respect. Rather, it measured levels of toxicity (damage to tissues).
The study concedes that proton therapy exposes sensitive heart tissue to less radiation than x-rays, but that wasn’t their focus. Had that been the focus, the headline would have been “Proton Therapy Exposes Heart to Less Damage than IMRT,” which I think patients would find extremely relevant. Instead, they were measuring radiation pneumonitis (RP), inflammation of the lung caused by radiation, and something called local failure (LF). After one year, the combined rates of toxicity were 17.4% for IMRT and 21.1% for proton therapy. X-rays win, or so it would seem. Hence the headlines. But not so fast. Let’s look a bit closer.
In order to compare x-rays and protons equally, they were given the same protocol, beaming from one side of the body. Lymph node also required treatment. Protons were required to reach the far lymph nodes by first passing through the tumor, the same way x-rays do, resulting in damage to surrounding tissue. Then, half-way through the trial, they realized identical protocols did not give a fair chance for proton therapy to benefit from its unique characteristic. It was being forced to act like x-rays.
With a new protocol, the protons were beamed precisely from each side of the lung. As usual, they stopped at the target. From that point forward, once the comparison was fair, protons vastly outperformed x-rays. I will give some numbers below. A rightful result would have been to report only the second half of the test, during which protons were properly configured. Instead, they added statistics for the first and second half together, hence penalizing protons.
Not only that, other factors handicapped proton therapy even more. For one thing, they used the original double scattering technology.
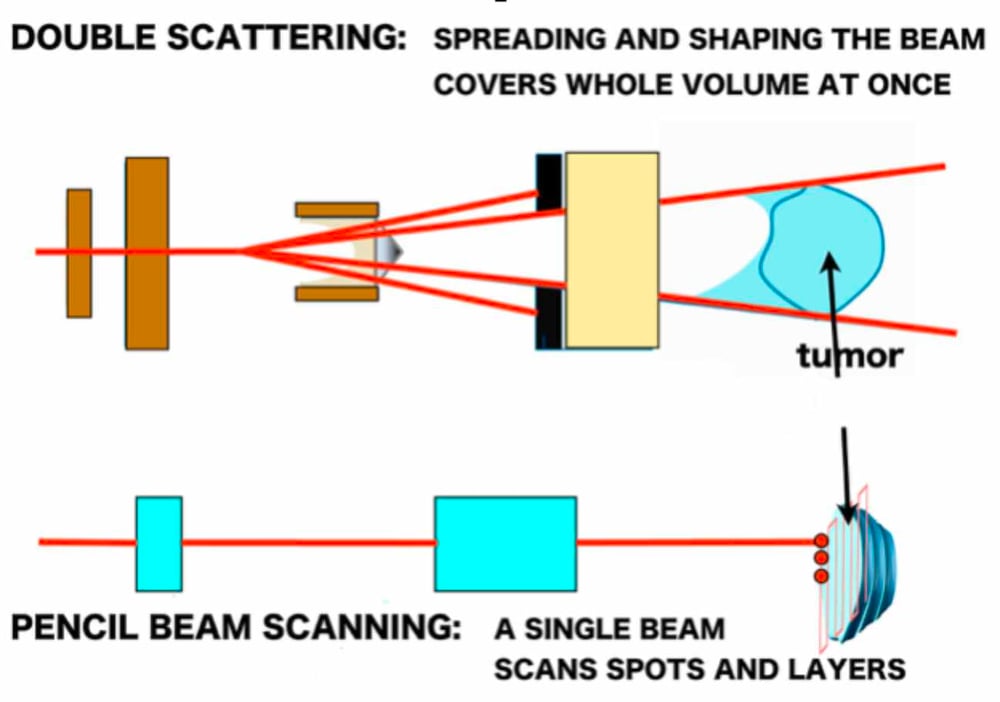
For a detailed explanation of the two technologies, see: PHYSICS.
If they repeated the trial today using pencil beam scanning, protons would again outperform x-rays, just as it did in this study, under far worse conditions. The trial took place in 2012 before the availability of pencil beam scanning, but reported in 2018, after pencil beam scanning was firmly ensconced. The purveyors of this study knew when they reported it in 2018 that it was outdated and did not represent current proton therapy capabilities. I consider that an act of desperation to find a study that favored x-rays.
This trial gained a lot of traction in the radiology world, frequently repeated as proof that x-rays have fewer side effects than protons. Stay with me now as we see some numbers and response from proton experts.
Breaking down the results a little more, we find that LF slightly favored proton therapy, 10.5% vs. 10.9% for X-rays. The crucial difference showed up in the RP inflammation factor. The highly acclaimed statistic for the entire year gave protons an RP rate of 10.5% vs. 6.5% for IMRT. Wrong.
Jeffrey Bradley, MD, director of the S. Lee Kling Center for Proton Therapy at Washington University School of Medicine in St. Louis, Missouri, responded to the treatment of the lymph nodes.
Their proton planning skills got better over time; the incidence of pneumonitis went to zero after trial midpoint, because they stopped trying to treat patients with contralateral lymph nodes where the proton dose was scattering to the opposite side of the chest.
The ability to stop at the target gives protons a great advantage. So going beyond the target to treat the lymph nodes on the opposite side did not utilize proton therapy’s unique characteristics and increased exposure to healthy tissue, causing RP. Improving their methods for proton therapy by treating the lymph nodes from the closest side reduced the incidence of RP to zero. Zero! Zip! Nada! The RP for IMRT stayed the same throughout the trial.
That bears repeating. After being properly used, protons cause no RP. Yet the report claimed protons did worse than x-rays. For the second half of the trial, x-rays remained the same. That was the best they could do. From the midpoint of the trial RP for protons equalled zero, and for x-rays, remained at 6.5%.
Here is Dr. Bradley again.
Let's say you had an ice hockey team, and you can't use your best skaters -- everybody on the team has to be able to skate at the same level. You know you're going to get a similar outcome. Almost all experts in proton radiation therapy feel like they handicapped themselves by that study design.
Proton therapy’s star players had to stay on the bench. The game was fixed. But there is more. Proton therapy suffered further disadvantages.
In addition, the targets were larger on the proton arm than they were on the IMRT arm. It was early in the proton experience and they were worried about missing the target so they enlarged their aperture. They ended up treating, circumferentially, about 8-10 mm wider around the tumor with the proton arm. We've learned not to do that.
An aperture shapes the radiation to conform better with the target. For prostate cancer, it generally follows the outline of the prostate.

In this trial, they made the aperture for protons wider than for x-rays by 3/8 of an inch, exposing more tissue by design! Even then, protons out performed X-rays in the second half of the trial.
To make matters worst, a review of this study bought into its results. Dr. Feng-Ming (Spring) Kong, MD, from the Indiana University School of Medicine, wrote an editorial about this study entitled “What Happens When Proton Meets Randomization: Is There a Future for Proton Therapy?” Just the title gives one pause, as if attempting to give this study greater status and importance.
Completion of this study is not trivial because the evaluation of the benefit of a new technology rarely has been done during the century-long history of radiation oncology practice. From the first uses of x-rays and radium for cancer treatment in the early 1900s, to kilovoltage (superficial) x-ray machines and the era of cobalt-60 and megavoltage two-dimensional treatment, to Linac-based three-dimensional conformal technology and the current widespread use of IMRT, technologies have been developed and implemented routinely in the clinic without randomized trials.
With no required trials! Yet radiologists demand it for proton therapy. She continued:
Whether a better planning technique such as proton intensity modulation (IMPT) or pencil beam scanning (PBS) would have generated different results is hard to predict.
No, it’s easy to predict. Then Dr. Kong caves in.
Personally, as a radiation oncologist, I would not recommend proton therapy for NSCLC outside a clinical trial setting until a clinical benefit is demonstrated in a prospective randomized study.
Here she joins the chorus of critics demanding high standards of proof which were not required for their own technology (x-rays).
In contrast to the largest retrospective study of patients from the National Cancer Database, this prospective randomized study failed to prove superiority of proton therapy.
In contrast to? She's saying that this trial came to a different conclusion than the large retrospective study she mentions. Let’s take a look.
The National Cancer Database was queried to capture patients with stage I-IV NSCLC treated with thoracic radiation from 2004 to 2012. A total of 243,822 patients (photon radiation therapy: 243,474; proton radiation therapy: 348) were included in the analysis.
On multivariate analysis of all patients, non-proton therapy was associated with significantly worse survival compared with proton therapy. On propensity matched analysis, proton radiation therapy was associated with better 5-year overall survival compared with non-proton radiation therapy For stage II and III patients, non-proton radiation therapy was associated with worse survival compared with proton radiation therapy.
The results from the National Cancer Database concluded that x-rays were “associated with significantly worse survival.” I would think living longer is rather more important than a bit of inflammation!
So, the reviewing doctor accepted the slanted results of this trial even though other studies clearly showed just the opposite, casting even more doubt on this study.
While claiming the false conclusion, Dr. Kong gives several reasons the results for the study may have been skewed against proton therapy. For example:
Finally, the study design in terms of endpoint definition, control of confounding factors, and dealing with the lung dosimetric restriction may have confounded the results.
Confounding factors are those which would throw off the results. For example, she points out they measured RP as “in-field radiographic changes.” That means around the tumor site. X-rays, however, affect much more tissue and could have produced RP outside of the targeted field that escaped measurement. Protons would be much less likely to have such effects. They simply didn’t measure a parameter likely to be unfavorable to X-rays. Nor were other important factors taken into consideration, such as which participants took chemotherapy drugs. This trial had some serious design limitations, lessening the likelihood of a fair conclusion.
More importantly, the study required patients to meet dosimetric limits for both the PSPT and the IMRT arms, which may have resulted in not being able to enroll patients who would most likely benefit from protons.
They eliminated the best prospects for proton therapy! Pardon my exclamation points. Going back to a sports analogy, if they take all the opposition’s best players off the field, they are more likely to win. Disappointingly, after noting these qualifications, Dr. Kong accepts the skewed results and gets political.
Although negative results from a phase II study in NSCLC cannot exclude the potential benefit of proton therapy in other clinical situations, such as for pediatric patients, and the cost of proton therapy will be significantly reduced by newer technological changes, this trial should at least cause some pause in hospitals that are building these facilities for competitive reasons and not for cost-effectiveness reasons.
Dr. Kong warns hospitals from getting proton therapy, based on the conclusion of this trial that she herself identifies as flawed and not typical of results found in the cancer database.
Varian, a leading manufacturer of both X-ray and proton therapy equipment paid Dr. Kong for writing her editorial. Frankly, I think she deliberately avoided taking sides, hinting that protons lost but perhaps unfairly so.
The study we have examined claims to be the first such randomized trial. Here is another trial stating it is the first prospective trial: https://pubmed.ncbi.nlm.nih.gov/28678434/
Want more? Here is yet another study favoring protons: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5960657/
Remember, these studies date back quite a few years. Newer ones, using pencil beam scanning, are even more favorable (unless designed to slant the results). Far from wanting to avoid comparison and scientific trials, proton therapy advocates encourage it, knowing that proton therapy will hold its own.
Can we assess the effect of this attack on proton therapy? Here are several examples, based on the questionable aura of doubt unfairly associated with proton therapy.
Cleveland Clinic, in Ohio, proclaimed it has no plans to get proton therapy. Dr. John Suh, chair of the Department of Radiation Oncology at the Clinic's Taussig Cancer Center, repeats the official mantra:
The reason we have not actively pursued proton beam therapy is that the number of indications and the evidence for the use of proton beam therapy is still lacking.
Misinformation served its purpose in limiting the advance of proton therapy to the Cleveland Clinic. Another center, planned in Baton Rouge, met the same fate when Dr. Rebekah Gee, the state’s health secretary, claimed there is “little evidence that it is effective.”
Not just equal, but effective at all. She questions whether it even works. Similarly, plans by Provision CARES for a proton center in New Orleans fell through when the original partner bailed out, citing the same reason.
Here is more fallout from fake news. Journalist Jay Hancock wrote a real hatchet job against proton therapy in Kaiser News, stating:
But (proton therapy’s) pinpoint precision has not been shown to be more effective against breast, prostate and other common cancers. One recent study of lung-cancer patients found no significant difference in outcomes between people receiving proton therapy and those getting a focused kind of traditional radiation, which is much less expensive. Other studies are still underway.
There you have a direct reference to the flawed lung study examined above. He used that faulty data to make his conclusion. Alas, the New York Times and other media reprinted his article, exposing it to millions of readers. Based on this biased result, many insurance companies felt justified in refusing coverage for proton therapy.
Finally, let me quote some snippets from other articles on proton therapy.
Dwight Heron, MD, chair of radiation oncology at UPMC Shadyside in Pittsburgh, said that for those men who do need radiotherapy,
we can do it just as well" with conventional treatment. Proton therapy "does play a role, but we don't have the clinical evidence yet to support the use of protons for the range of cancers we usually treat—and certainly not at the current cost.
Note that many of the critics of proton therapy and defenders of x-rays are traditional radiologists working in facilities that do not have proton therapy, as above. Yet even he admits proton therapy is "unequivocally better than conventional therapy in terms of morbidity and outcomes.”
Oh, that’s all. Protons are only better regarding side effects, quality and length of life. Well, who would care about such minor advantages? (Pardon my sarcasm.)
Whatever effect plasmas and protein (sic) beams might have on cancer, they were evidently not having the hoped-for effect on patients.
Plasmas? Protein beams? This makes no sense.
If proton treatment centers each treated 500 patients per year, there should be enough patients to support 100 centers across the country. Why, then, are so many of them facing such harsh economic realities?
One reason is that insurers are not covering most proton therapy. But the other explanation is the disturbing one: Radiation oncologists don't want to give away their income-producing patients.
"No provider is willing to give up patients, even though they know the long-term toxicity and morbidity of the patient they are treating with conventional therapy is bound to be higher.”
Did he really mean that oncologists would knowingly give patients sub-optimal treatment for financial reasons? Absolutely, he said. And they're unlikely to be exposed, because "they can always claim that they don't know."
He said he's seen it happen."We had a proton facility at Jacksonville and a main campus in Gainesville. Our radiation oncologists in Gainesville would not send patients to Jacksonville. They would make the excuse that 'there's no evidence that protons are better. So why put the patients through a 70-mile drive [to Jacksonville]?'" This was not a question of competing institutions fighting for healthcare dollars. It was a civil war: both the Gainesville and Jacksonville facilities are part of the University of Florida.
Finally, after discussing the cost of proton therapy, several authors made these conclusions:
"It could bankrupt the healthcare system even more quickly."
“Could this change as researchers continue to study proton therapy? That's highly unlikely. The physics is simple. We know which cases will make a difference."
"It's personalized medicine at $220 million a pop.”
When I read statements and conclusions like these, it makes me think of buggy whip manufacturers saying cars were just a fad, they were too expensive, and they didn’t do well on dirt roads. Horses and carriages are definitely the way to go.”
GO BACK TO PROTON PAGE
GO TO HOME PAGE