My Experience with Proton Therapy
Once diagnosed with prostate cancer, I didn’t just do whatever my doctor told me. That has been a strong pattern in my life, that I have been proactive when it comes to my health. I researched and read books and made my own decision. Once I was at a proton center being treated, I discovered that 85% of the men there had been self-referred, meaning they made their decision based on their own research and efforts.
I read several personal accounts of men treated for prostate cancer with proton therapy. That was helpful, but when I finally experienced it firsthand, I found my experience varied from theirs in many ways. Yet even with different technologies, different procedures, and different approaches, the similarities and results were quite convincing. The significant aspects of my experience include:
<> Getting 80% of my treatment (then not covered by United Healthcare) paid by being on a Medicare registry.
<> The use of a hydrogel spacer to protect the rectum meant no daily rectal balloons.
<> The accuracy of my PSMA scan identified cancer not detected in the MRI scans, which changed my whole treatment protocol. This is a game changer. If you read nothing else, scan to the portion of this essay discussing PSMA.
<> For the first time I had a medical physicist and dosimetrist.
<> I was so impressed that from the very beginning I made an effort to document all aspects of my experience.
So here is my story.
I was lax in paying attention to my rising PSA, and to my dismay, so was my (former) family practitioner. Here’s what they were.
February, 2013: 3.15
January, 2015: 6.46
July, 2015: 6.40
January, 2016: 12.3
May, 2016: 16.0
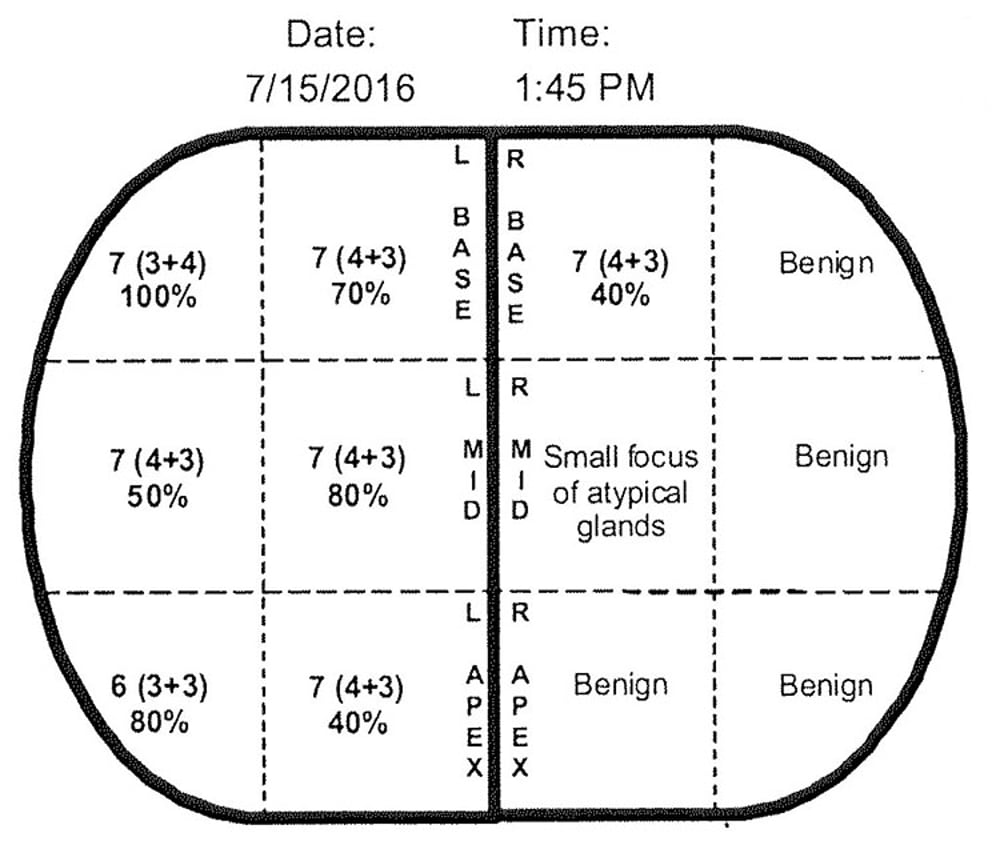
In January, 2016, I changed health plans and doctors. The routine blood test showed a PSA of 12.3. Over four ensuing months we investigated non-cancer causes, which didn’t pan out. By May my PSA was 16.0 and I went to see a urologist. He was woefully out-dated in his methods, but did a skillful (if old fashioned) job on the biopsy. It showed cancer in seven of 12 core samples, as shown below. My Gleason score was 4+3=7.
I had a bone scan that showed no metastases. However, it showed a problem in my jaw. I went to my dentist who discovered a serious abscess, leading to a root canal. I had an MRI and was relieved that it showed no cancer outside of the prostate gland. This would turn out to be wrong, as you will see a little further on.
When I asked about proton therapy, both the urologist and the surgeon I visited gave me misleading and erroneous information. It could have been caused by ignorance, or an attempt to lead me to get my treatment from them, or perhaps a result of some bias against proton therapy. None of those possibilities are very good, whether being ignorant, misleading, or unethical.
Therein lies my number one piece of advice:
DON’T RELY ON YOUR DOCTORS FOR ACCURATE INFORMATION ABOUT PROTON THERAPY.
It reminds me of the story of the man who died and went to heaven. There, he saw a figure dressed in a long white jacket carrying a stethoscope around his neck, going around examining people. “Who is that?” the man asked one of the angels. “Oh,” said the angel, “That’s God. He thinks he’s a doctor.” The point being many people treat their doctors as if they are infallible, blindly following their advice. That can be especially unfortunate when it comes learning about to proton therapy. At the very least, become informed by reading this website and following some of the links to further material. Better yet, get a second or third opinion, preferably from someone at a proton therapy center.
Realizing that my insurance would not cover proton therapy, I called around to various proton therapy centers to ask the out-of-pocket cost. I had read of men who mortgaged their homes to pay for proton therapy. I thought about going abroad, as there are centers in Korea, Prague, China, India, and elsewhere that charge much less than in the United States. Most centers wouldn’t give the cost over the telephone. The University of Florida quoted a special cash price of $134,000.
On August 8, 2016, Samantha at Provision CARES Proton Therapy Center in Knoxville, Tennessee (now called the Thompson Proton Center), gave me their price, for the same treatment with newer equipment, which was $93,000. It pays to shop around. Then she asked the question that made all the difference: “Are you on Medicare?” I assured her I was.
She told me if I agreed to be on a Medicare registry that tracked the results from my proton therapy, Medicare would pay for 80% of the cost of my treatment. I was skeptical. That would be too good to be true. So she put me in touch with Steve in the finance department who assured me that if I would take part in a registry to track the results of my proton therapy, Medicare would cover 80% of my cost for proton therapy.
What would I have to do? Every six months for the rest of my life I would get a blood test to check my PSA and an exam from my doctor, reporting the results to the registry. That didn’t sound like a burden and so that’s what I did. Then, United Healthcare agreed to pay the remaining 20%.
I pursued the possibility of going to Knoxville for two months for treatment. The medical director, Dr. Marcio Fagundes (now at a proton therapy center in Miami), answered my questions and explained the protocol. I overnighted copies of my bone scan and MRI. The financial and insurance departments got all of my personal details. Only one problem developed.
Dr. Fagundes wanted me to take hormones for several months before getting treated. I didn’t want to do that. Androgens, mainly testosterone, feed prostate cancer. Hormone therapy deprives or suppresses these androgens, making the tumor(s) shrink and become much less active; therefore, easier to treat. The testicles produce most of a man’s testosterone. Surgically removing them (castration) solves the problem. However, castration would be irreversible with permanent side effects. Hormones achieve chemical castration, reaching the same goal, but one can stop taking them and end the side effects. Hormones don’t kill cancer; they just delay its growth. After a few years, hormones stop working as the cancer becomes resistant to them.
Luperon was the hormone of choice. The potential side effects include fast or irregular heartbeat (I already have that), sudden decrease in blood pressure, blurred vision, joint pain, unusual bleeding or bruising, cough, diarrhea, loss of appetite, runny nose, shivering, insomnia, erectile disfunction, and more. Whew! Samantha told me she herself had taken Luperon for breast cancer and had no trouble other than hot flashes. Dr. Fagundes told me in the long run, the difference between using hormones or not affects the survival rate by a couple of percentage points. I was willing to take that risk. Even though hormone therapy is standard practice, they agreed to proceed without me having to do it. I have since met men who wished they could have avoided it and simply accepted the increased risk of recurrence.
Within two weeks of my first contact with Provision, Linda and I drove from San Antonio to Knoxville to begin my treatment. She was with me every step of the way, truly a shared vision. We rented a cute little bungalow for two months, an easy drive from the proton center and near Whole Foods, restaurants, and the public library.

My first day, September 1, 2016, was a very busy one. I received my ID tag (photo). I filled out and signed many documents. A nurse took my blood pressure, which was 159/93. I guess I was stressed out. My preparation had actually started a week early with changes in my diet to avoid flatulence, which can cause the prostate to move. Before they could get started, I need to give myself an enema, for which I used a Fleet bottle. My full-length book about proton therapy for prostate cancer goes into much more detail, some of it quite humorous.
They gave me a Valium to relax me, Hydrocodone/Tylenol for pain relief, and an antibiotic. They also applied EMLA numbing cream to the perineum area. It became eminently clear to me that treatment in this part of the body quickly divests you of any sense of privacy or embarrassment.
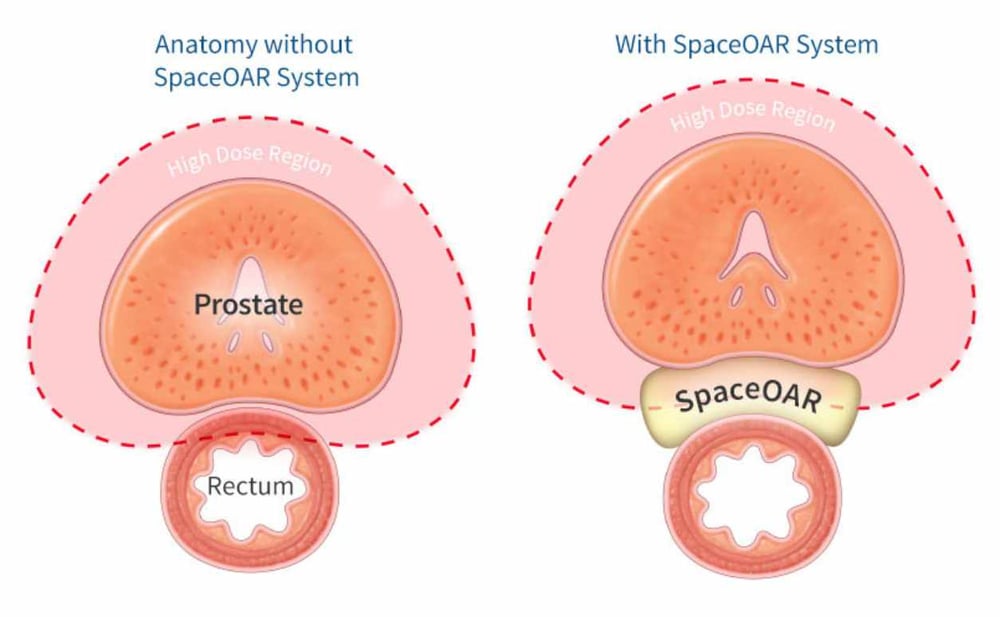
Dr, Fagundes performed two medical procedures. He inserted three gold fiducial markers in my prostate, which would help line up the equipment (x-rays, protons). Next he injected a hydrogel called SpaceOAR which had been approved only weeks before, but was not yet covered by insurance. OAR stands for “organs at risk,” meaning healthy tissue. It would provide a space between the rectum and the prostate, sparing the rectum from damaging exposure to radiation. See illustration below.
The alternative to hydrogel is a balloon that they insert into the rectum and then fill with water. This serves to stabilize the prostate so it doesn’t move. Since I was to have 39 treatments, the thought of 39 rectal balloons was not pleasant, although many of the accounts I had read by men who experienced balloons seemed to take it in stride. Some 20 years ago, Robert Marckini received proton therapy for prostate cancer in Loma Linda, California. Afterwards, he started an organization called the Brotherhood of the Balloon, or BOB. That organization has grown to nearly 20,000 members and has very informative materials and newsletters (see LINKS section). They could change their name to Brotherhood of the Beam and still be BOB.
I chose the gel, at a cost of $3,000. Now, I understand, insurance covers it. Perhaps I could start the Brotherhood of the Gell, or BOG. The procedure to inject the gel took about five minutes, which I found quite unpleasant, but the discomfort went away in a few minutes. It was the only time during all of my treatment that I felt anything. While the balloon stabilizes the prostate, it also pushes the rectum right up against it, assuring that it will receive some of the radiation resulting in possible bowel issues (colitis, etc.). Thanks to SpaceOAR, I had no issues or side effects. During the next two months, I received CT scans on several occasions to check the location of the gel and fiducial markers. They remained properly in place.
The next day we continued the preparations for my treatment.
I returned to Provision for two scans, first an MRI then a CT. One hour before the Computed Tomography (CT) scan, I emptied my bladder and drank a sixteen-ounce bottle of water. This would be the procedure prior to all of my treatments. They had me lie on the treatment table with my legs in a soft material that turned into a mold. By lying on the table with my legs in the mold, I would always assume the same position.
But there was yet one more precaution. They made two dots on my thighs, permanent tattoos,. which were where the nozzle of the proton therapy gantry should point. Having my first tattoos, I had to fight the impulse to go out and get something pierced.
Above: The technicians used a ballpoint pen to circle the tattoo for the above photo, which they took for me. They answered all of my questions and took photos, cooperating with my efforts to document my experience. I don’t know of any other book as detailed as mine, with actual photos taken during the treatment.
All of this preparation is called simulation, setting up the procedures to assure accuracy for the proton radiation. Proton therapy, while known for 70 years, didn’t proliferate until scanning and software improvements developed. Scanning will be covered later in this essay. Planning software is quite impressive. Provision chose Ray Station, designed by a very progressive company in Stockholm, Sweden. Using scans taken during set-up, the physicist manually traced my various internal organs on the screen. His training and experience resulted in great expertise in doing this. Once he traced the organs with different colors, the image could be moved and rotated to any angle. He showed me a side views from the side, front, and top. The computer calculates exactly the right direction from which the protons should be scanned and the depth they should reach, considering various scenarios to find the best one.
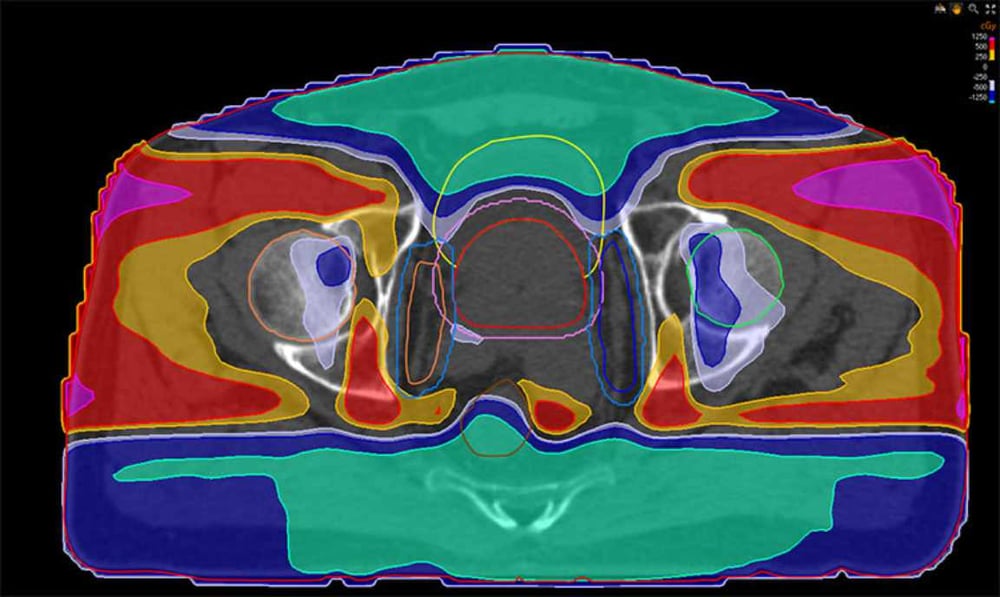
Above: A computer analysis of where the radiation would be the greatest (blue is the least, red is the most).
Pencil beam scanning, as previously described, covers the target in rows and layers of tiny overlapping spots, starting at the farthest point away from the nozzle and moving to the closest point. For thirteen treatments I had sixteen layers and 1,962 spots. Then, when the lymph nodes and seminal vesicles were added, it called for thirty-two layers and 5,276 spots. One article I read says that PBS lays down 400 spots per second, which means my treatment would take just over 13 seconds. During the planning stage, a twenty-two-page document mapped out every layer and every single spot. Hence the importance of computer software. Now, they are adding artificial intelligence to the mix for even more precision.
Typically, we arrived at Provision two hours early on most days. The lovely industrial park in which it is located offers walking trails, a flowing stream, pools, and more. After a vigorous 20-minute walk, we went to the fitness center across the street, where I would work out and Linda would take yoga classes. Afterwards, I timed my shower to end one hour before treatment time, emptying my bladder and drinking my bottle of water.
Next we went to the expansive and comfortable lounge area to wait for my treatment time. We sat at a table, read the morning paper, checked our email, and otherwise occupied ourselves.
A technician came for me and led me to the Autumn changing room where I shed my clothes and donned a typical backless gown. As I entered the treatment room, one tech asked my birth date. “July 21, 1944.” Then, I walked over to the table, stepped up on the footstool and swung my bare butt onto the clean white sheet. The table is hard, because cushions would cause unwanted movement. I snuggled my legs into the cradle, assuming the same position as during the original simulation.
The techs rolled up my gown from the sides and placed it on top of my legs, exposing my thighs but covering the genitals. One on each side of the table, the techs pulled on the sheet to move me in one direction or the other until the laser crosshairs lined up with my tattooed dots.
Photo: I was not in a circular gantry. Rather, the nozzle for the proton beam was in a fixed position. You can see the crosshairs on my thigh.
There was much more to assure accuracy than crosshairs and leg cradle. Next, the relevant equipment came out and took an x-ray of me on the table. The technicians had three screens in front of them: On the right was my original CT scan from the simulation and on the left, the digital X-ray that had just been taken. The middle screen superimposed both images, which had to line up exactly.
Then, they made sure the fiducial markers properly lined up. Their screen showed three areas with colored lines—one red, one green, and one blue—called the “grapes.” The three fiducials must fall within their grapes in both directions. Sometimes, to accomplish that, the computer minutely adjusted the table position, thereby assuring precision within two millimeters variation (the thickness of a quarter coin).
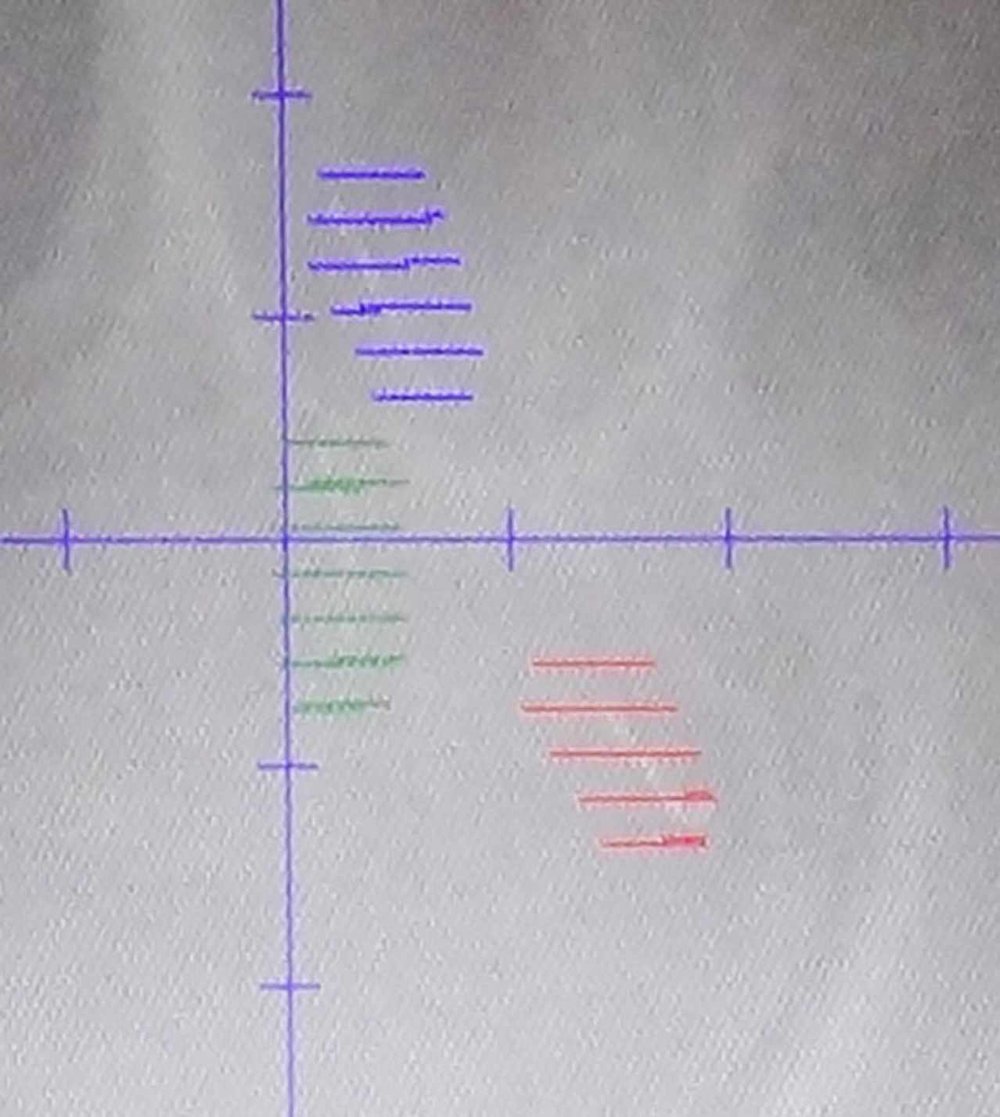
Photo: You can see the white lines of my fiducial markers lie within their appropriate grapes.
Satisfied with my positioning, the technicians returned, rolled away the X-ray equipment and said, “Here we go.” I didn’t move an iota. To occupy my hands, I held a round rubber circle called the steering wheel over my chest. They then used a handheld barcode scanner and scanned barcodes on my table, my leg cradle, the nozzle, the degrader, everything (six or seven items). If anything didn’t match, an alarm would sound and the proton equipment would not function.
A bell sounded, meaning everyone must leave the room (except me of course). The techs exited by the same doorway through which we entered earlier. Protective doors closed first. Then a massive 60,000 pound (thirty-ton) door five feet thick, made of very dense concrete, rolled closed, half from each side. The walls are even thicker, giving protection from errant neutrons. The techs kept an eye on me on the monitors in the control room.
Beyond even these extensive procedures, there are other efforts made under the category of quality assurance. For example, every day my oncologist would look at the x-rays to double check the technicians. Even with these precautions, something could change. The hydrogel could move, the tumor might shrink or change shape, the patient can gain or lose weight.
Technicians check on the quality of the proton beam itself. It passes through three consecutive ion chambers at the treatment end of the beam line which measure the beam. One time, there was about a two-minute delay while I was on the table. I asked what had happened. The tech said the beam had gone out of calibration. Elsewhere, in a control room, engineers made a quick adjustment and everything then proceeded according to plan.
Our stay in Knoxville was very vacation-like. We checked out nearby Gatlinburg and Pigeon Forge, visited friends in Lexington, Kentucky, and had a fine time at coffeehouses and restaurants. We began on September 1 and finished my last session on November 1. Before driving away, we had a small ceremony in the lobby which involved saying a few words of thanks and ringing the victory bell.
The custom of ringing a bell presumably started in 1996 when Navy admiral Irve LeMoyne neared the end of his cancer treatment. He told the doctor he wanted to ring a bell when the job was done, which is a Navy tradition.

After ringing the bell, we jumped into the already-packed car and headed home. My total cost, including the SpaceOAR, lodging, meals, gas, and everything came to $12,000. That’s getting away pretty cheap. Except I didn’t.
CANCER RETURNS
I duly followed the requirements of the Medicare registry, seeing my doctor every six months and monitoring my PSA. From a pre-treatment high of 16.0, three years post-treatment my PSA reached a low of 0.30. Then it started to go up again. I was hoping it was a fluke, but it continued to rise. By summer, 2021, it reached the threshold for diagnosis of recurrence, which is two points over my previous low, or 2.3. I needed to do something.
How to treat recurrence is a controversial subject. The plan of action depends on many factors, such as age, health, prior treatment, and personal preference. A common response is hormones, which I had previously avoided. Perhaps that is why the cancer returned, I thought. Had I made the wrong decision? I researched alternatives to hormones (androgen deprivation therapy, known as ADT).
In the United Kingdom, they have been doing clinical trials showing that estrogen can reach chemical castration quickly. While not without its own side effects (including the development of “man boobs”), estrogen avoids the serious consequences of pharmaceuticals used for ADT. They have investigated administering an estrogen gel to the skin, rather than taking it orally. This method of administration avoids severe side effects. However, when I searched for any such clinical trials currently taking place in the US, I couldn’t find any. Once again I considered going abroad if necessary.
Treatments depend on the nature of the recurrence. If the cancer has metastasized, then a local treatment is no longer possible and a systemic one, such as ADT, is called for. A more ideal circumstance is for local recurrence, in which the cancer remains within the boundary of the prostate. Then, various local treatments are possible, such as cryoablation (freezing the prostate to 40 degrees below zero), HIFU (using high frequency ultrasound waves to destroy the cancer), brachytherapy (radio active killer seeds placed into the prostate), and more. I, of course, looked into all of these.
I also wondered what had gone wrong the first time. I thought of several possibilities. Perhaps the dosimetrist made a mistake in drawing my internal organ locations for the Ray Search software. Maybe the technicians didn’t line me up right. Perhaps the quality assurance had failed. These were very depressing possibilities. They threatened to lower my exultant view of proton therapy. How could I promote books and websites about a technology that had actually let me down?
I decided to get three opinions regarding my options. Two suggested getting a fusion biopsy followed by cryotherapy (freezing the prostate to destroy it). I favored skipping the biopsy altogether and going right to MD Anderson for cryotherapy. In fact, I contacted a doctor there who had been highly recommended. But first, there was one more factor to consider.
PSMA - A Game Changer
I had been trying for two months to get a PSMA scan. At that time, only the University of California in Los Angeles and San Francisco had been approved by the FDA. I had my family doctor send an order for a PSMA scan and I called and left messages on the internet, all to no avail. They never responded.
PSMA stands for Prostate Specific Membrane Antigen. Remember that PSA, the blood test for prostate activity, stands for Prostate Specific Antigen. That antigen is very specific to the prostate. Even if the cancer spreads to other parts of the body, it is still prostate cancer. The PSMA scan combines a drug that goes directly to prostate antigen with a radioisotope that shows up as a bright light on a PET/CT scan. The scan can detect cancer as small as two millimeters, much more accurate than an MRI.
I tried to get a PSMA scan by joining a clinical trial. The best candidate seemed to be Oregon Health and Science University (OHSU) in Portland, which had just been approved by the FDA to offer PSMA scans. They used the radiotracer [18F]DCFPyL), which has a brand name of “Pylarify” (see www.pylarify.com).Several weeks passed and they did not call me to schedule a scan.
Finally, I received a call from Knoxville telling me they could perform PSMA scans. I made my appointment on the spot. Linda and I flew to Knoxville so I could receive the scan. The day of the scheduled scan I received a call saying it would be delayed by two days because the dose had not passed quality control. Finally, on September 1, I received the scan. They injected the isotope into my veins, after which we waited an hour for it to spread throughout my body. Then they did a CT scan. The next day, I met with the doctor to discuss the results. This is where the story turns miraculous.
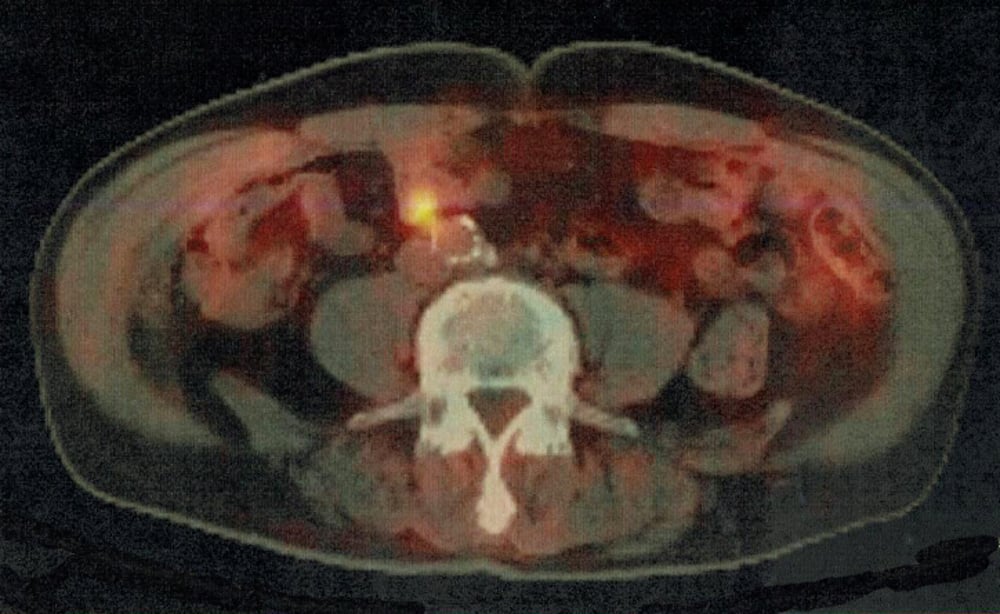
Above: On the PSMA scan, the cancer lit up like a Christmas tree. The cancer was not in the prostate or areas previously treated.
My oncologist informed me that the original proton treatment had been flawless. There was no cancer there at all. However, a few cells of cancer must have escaped from the lymph nodes, or were already there but undetected by the MRI, and settled in the abdomen lymph just above the previously treated area. I would again qualify for proton therapy.
My previous assumptions proved to be completely wrong. What if I had gone directly to cryotherapy to destroy the prostate, when that was not the correct location! I sent a scan to my family doctor for my medical record. He had misread the MRI as well.
The fact is, nobody got it right until the PSMA scan showed the new area of prostate cancer. In 60% of the cases, PSMA scans result in a revised prognosis and changed treatment plan. No man with prostate cancer should proceed with treatment until receiving a PSMA scan. There are several YouTube videos about PSMA. Here’s one I thought was well done: https://www.youtube.com/watch?v=MifLWOxj990
Note these key points about PSMA scans:
1. It is as much as 250% more accurate detecting cancer not visible on MRIs.
2. It detects cancer at an earlier stage when it is still minimal or the PSA has not gotten very high.
3. In two-thirds of the cases, the result of the PSMA scan changes either the diagnosis or the treatment plan, or both.
Linda and I again spent two months in Knoxville, in 2021, five years after my previous treatment. Because housing was unavailable, we stayed in a hotel. Due to COVID-19 we did not travel much and ate only at restaurants with outdoor patios. This time around we knew just what to expect. Once again I refused hormone therapy. Once again I had no ill effects. Once again we drove back to San Antonio greatly relieved, stopping at Cracker Barrel restaurants along the way.
I remain extremely positive about proton therapy. However, my advancing age and limitations on time and money have caused me to downsize my websites. However, I give many links for further information. If you want to hear more from me, here is a link to my book, available on Amazon (this is not a purchase link):
https://www.amazon.com/Prostate-Cancer-Conquered-Proton-Therapy-ebook/dp/B083CSJLW1
Note: The above link goes to the kindle electronic version, for $7.95. If you have a black-and-white kindle, I suggest getting a free kindle app for your iPad or computer. On it, all of the illustrations will be in full color.
HOME PAGE
MAIN PROTON PAGE